Sore eyes after cataract surgery
Cataract surgery for most people is a relatively pain free experience. After the surgery some mild scratchiness or soreness and foreign body sensation is to be expected for a few days – I usually tell patients that this ordinarily settles within a month or so . For some people, the surface discomfort persists up to 3 months and for a tiny minority up to 18 months. It would be uncommon for it to last longer than this.
So, what are the reasons for excessive surface symptoms and what do we look out for? Here are some of the pointers:
Check for post operative iritis and for raised intraocular pressure. Whilst these aspects do not cause soreness in themselves, we do need to make sure they are treated. Also look at the cornea carefully – I have seen on occasions post op viral keratitis such as adenovirus and herpes simplex ulcers.
Some eye ache is very common for up to 3 months, particularly in young people, as the ciliary muscles try to pull against the (immovable) lens implant. The eye tries to accommodate and can’t do so. It adapts over 3 months and the aching settles in that time.
Dry eyes are the most common factor and, in fact, so normal that I tell everyone that all eyes are drier after surgery for up to 3 months. It is best to pretreat for at least a week pre op with blepharitis control and tear drops to optimise the ocular surface environment prior to the operation.
To treat the post-surgery dry eyes, any tear drops may be used. Preservative free tears are often better if possible. They can be started any time after cataract surgery but often easier for many patients after the post op drops are reduced. They are already taking a lot of eye drops after their operation.
(There seems to be a trend in some clinics and hospitals to reduce the number of weeks and reduce the frequency of post operative eye drops for cataract surgery. One clinic recently has been promoting not using eye drops at all (and just giving steroid and antibiotics at the end of the operation). In my experience, more patients come back with more serious problems from insufficient post operative eye medication rather than those who have problems from the drops and the regimen. Issues with post operative drops can be remedied straightforwardly but problems with recurrent iritis or inflammation after surgery are trickier and more of a risk to sight and more of a risk for extended post operative recovery).
Some stinging from the post-surgery drops is very common – especially with drops such as Tobradex and Acular. This can be remedied by changing the drops if needed. If the eyes become more red and or more sore then there can be allergy to the medication or preservatives in them and, again, usually remedied by changing to a simpler preservative free drops regimen.
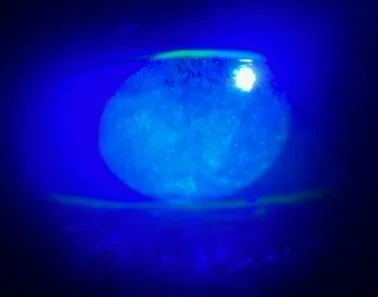
Image left shows corneal staining from drops toxicity post cataract surgery having a significant impact on vision.
There are, of course, cuts on the surface of the eye for the surgery. These, in themselves, change the smooth contour of the surface of the eye and that changes tear distribution giving more dryness and there can also be a foreign body sensation from the grooves and ridges of the cuts themselves. The wounds smooth over usually within a month or so but on occasion can produce a ridge or dip which can be seen with fluorescein staining and need a longer course of post operative tear drops over 3 to 6 months. Do vitamins C and E help wound healing? Potentially. It is worth mentioning this to the patients who are having above average ocular surface symptoms. I have no problem with them taking vitamin C 2000mg daily orally for a month or so.
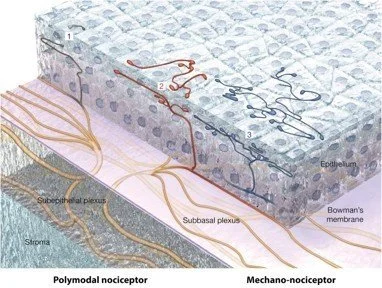
Ocular neuropathic pain: this is not just any eye pain - it is excessive pain or discomfort above what would be normally expected in the absence of significant clinical findings. It used to be called ‘pain without stain’, ie painful eyes in the absence of significant dry eye or other findings visible at the slit lamp. It can occur in patients with dry eyes but also can occur post surgery especially in patients who have had previous lasik and more so with some personality types. The pain sensation can be created in the nerves in the cornea but also sometimes centrally ( in the brain) or can be a combination of both.
Patients who perceive severe ocular neurpathic pain after cataract surgery are often very analytical and anxious; perhaps with a history of depression or variable emotional state. They seem to research every aspect of surgery and how it is done - on the internet and from friends and family. They analyse each symptom and try and pinpoint a cause and solution .They are looking for something that is not right so they can understand it and fix it or find an explanation. The problem of course is that there are often multiple reasons, most of which are harmless and nearly all of which settle completely over time. The problem is that this sometimes becomes an obsessive pursuit and the more they think about their eye symptoms the more the symptoms become amplified and prolonged. The conclusions that they reach are often overly simplistic and not correlating with the medical status of the eye. These individuals need a lot of time to go through every concern and conclusion that they have reached and often need an early second or third opinion for reassurance ( which they still may not agree with). They also need multiple tests and scans at intervals them that all is fine and that nothing has technically gone wrong and lots of assurance and reassurance that the discomfort will get better. Multiple appointments at regular intervals over 18 months are usually needed but also the optometrist and ophthalmologist needs to review their own findings from time to time so as not to miss any other treatable cause. Oral treatment with amitryptiline has been advocated – this is not something I have given but I do find that in these very infrequent cases that a course of topical non steroidal anti inflammatory drops such as Voltarol Ophtha, Bromofenac Nevanac or Acular can help– I give twice daily for at least two months.
Blepharitis, of course, can give secondary surface symptoms. The best option is to ensure that the eyelid inflammation and oil secretions are as minimal as possible pre surgery. A course of compresses and tea tree oil wipes for a couple of weeks pre op is always good. Oral omega supplements such as flaxseed capsules 2000mg daily can help, as can a course of oral tetracyline ( is there Rosacea?) pre operatively for one month. Some patients can also benefit from a course of Intense pulse light therapy to the lid margins to calm the lids down.
When can patients start their lid hygiene regime post operatively? I would avoid any compresses or wipes for at least four weeks. I had one patient in early 2025 present with acute pain and reduced vision one morning two weeks post cataract surgery. The concern was whether there was an acute infection or very high eye pressure but when seen there was a large corneal abrasion and folds in the Descement membrane layer in the cornea. These findings can occur post surgery with blunt trauma and rubbing the eye. This patient denied any trauma so we treated with topical lubricants and anti-inflammatory drops. Two months later the patient asked me if the microwave eye bag she had put on the eye at bedtime could have had any relation to the event? We then had an answer to what had happened!
Corneal abrasions can happen from the tips of the eye drop bottles and can happen more easily in patients with corneal dystrophies and unstable corneal epithelium ( sometimes the epithelium can just start peeling off during surgery) and also in patients with a history of recurrent corneal erosion syndrome caused by trauma years before. These patients at risk of abrasions should be counselled pre surgery and given more ocular surface lubricants both pre op and post op.
Do also keep checking for foreign bodies on and around the eye if the patient is feeling uncomfortable. Conjunctival concretions, ingrowing eyelashes and eyelid entropion all seem to have a habit of becoming more manifest at a time when you don’t want them!
Whilst we are talking about eyelashes – do look out for them ! When operating sometimes lashes fall out – either spontaneously or from the glue from the drapes. Usually we see them early on during surgery floating around the eye and we fish them out. Occasionally they are not seen as they can float and then get stuck deep in the recesses of the conjunctival fornices and pop out or work themselves out days and weeks afterwards. I had not seen any eyelashes causing problems for quiet a long time and then they come along in three patients.
The first was one who called in post op and said he was convinced he could see the lash in the corner of his eye . At least his vision was good after the surgery! I looked and yes there was a lash stuck vertically in the lower inner nasal corner of the conjunctiva standing vertically like a plant in a flower pot and so very easily just pulled out.
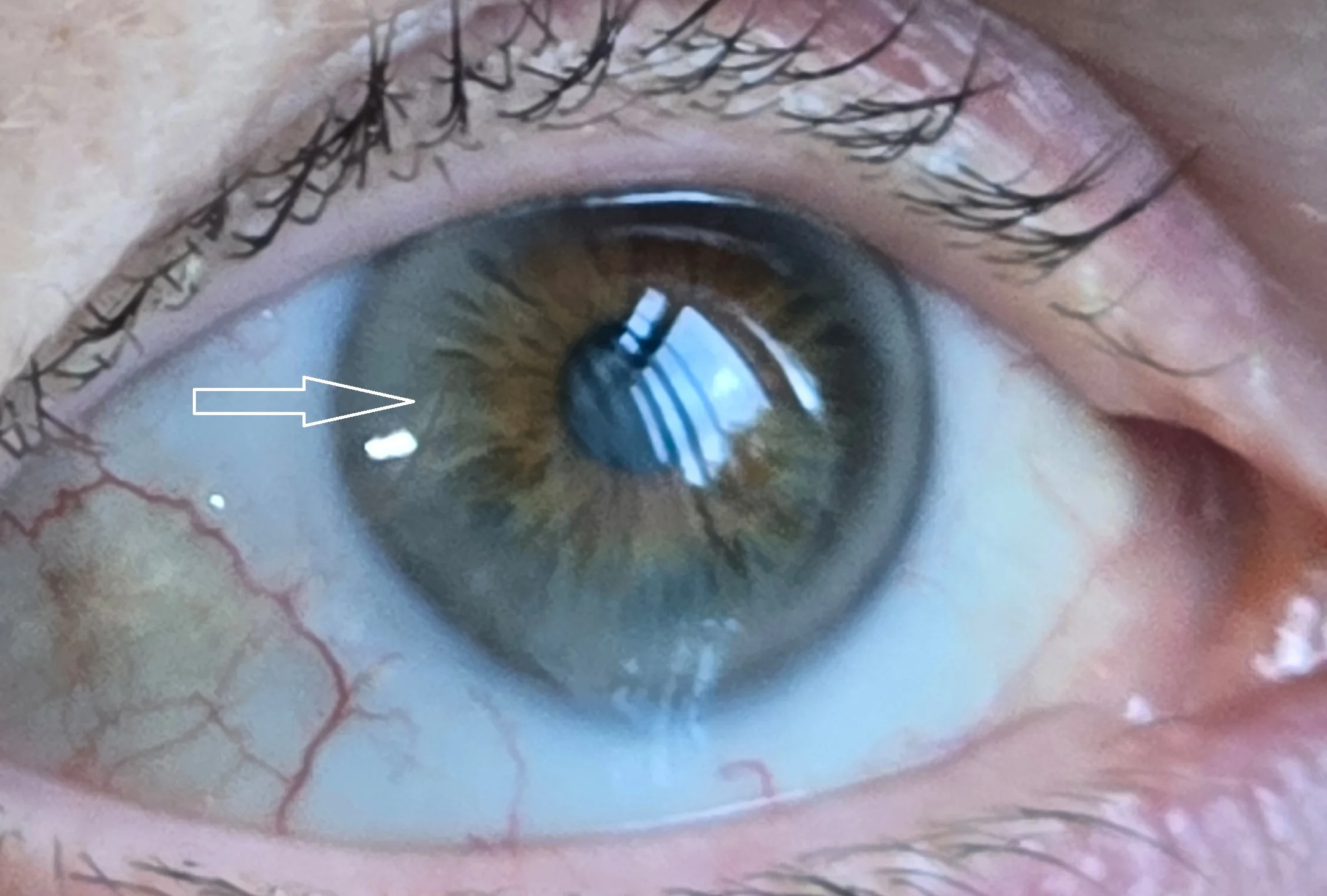
The second patient had recurrent redness and foreign body sensation for a month post cataract surgery and was seen by two other people before me with no findings. I saw the patient and, low and behold , an eyelash sitting just below the cornea in a horizontal line just under the conjunctiva. It must have been buried quite low in the fornix and not seen before and then migrated upwards. I gave some topical anaesthetic and scored the conjunctiva over the central 2mm with a needle – just as you would with splinter – to expose the middle of the lash and was able to pull it out smoothly without breaking it.
Have you ever seen an eyelash in the anterior chamber of the eye? I have. I saw one once when I was a junior doctor . My consultant showed me a patient who had undergone cataract surgery a year previously and had an eyelash sitting in the anterior chamber. Quiet. Asymptomatic. No inflammation. No infection. No redness. No effect on vision. Nothing. Just sitting there. The question we were asked was whether we should go back in and remove it. I voted for removal as the patient was only 50 years old. I don’t know what happened after that as I moved to another hospital.
Well, 28 years later I now have seen another patient with an eyelash in the anterior chamber and – yes – this time it was a patient I had operated on. What a surprise at the post op check! Again asymptomatic and no inflammation or redness but I elected to remove it as it was just in the wound internally and could have acted as a wick for infection to enter the eye. It was again straightforward to pull out by scoring the edge of the would and catching the edge of the lash to pull it out. Fortunately, it did not break or float away from me into the anterior chamber! I gave some intraocular antibiotics and all was well.
These were just some of my thoughts and observations for those of you seeing patients after cataract surgery who are having symptoms of soreness and discomfort. I hope you have found this useful.
Sundeep Kheterpal
May 2025